Our Director of Quality Anna Burhouse shares eight simple techniques for how to improve patient focused care in any organisation…
I have been working with the University of Bath to design a free Future Learn course on Quality Improvement (QI) for healthcare professionals. It has now run twice and goes live for a third time in May. Over 7,000 people have taken part and I have felt particularly moved by how much people shared about their own experience of being a patient, family member or carer and their observations of the health and social care systems they found themselves in. It was a really rich source of examples about how important it is to have person-centred care and how we must have patient experience at the core of our improvement efforts.
I also enjoyed the discussions about how to be an improvement leader in your local team, no matter what your formal role is in an organisation, especially the need to ‘walk the talk’ and demonstrate through personal actions the improvement you want to see manifested in the organisation. All of this made me think about some simple practical ways that we, as improvement leaders, could use to encourage a culture where patients are at the heart of our health systems.
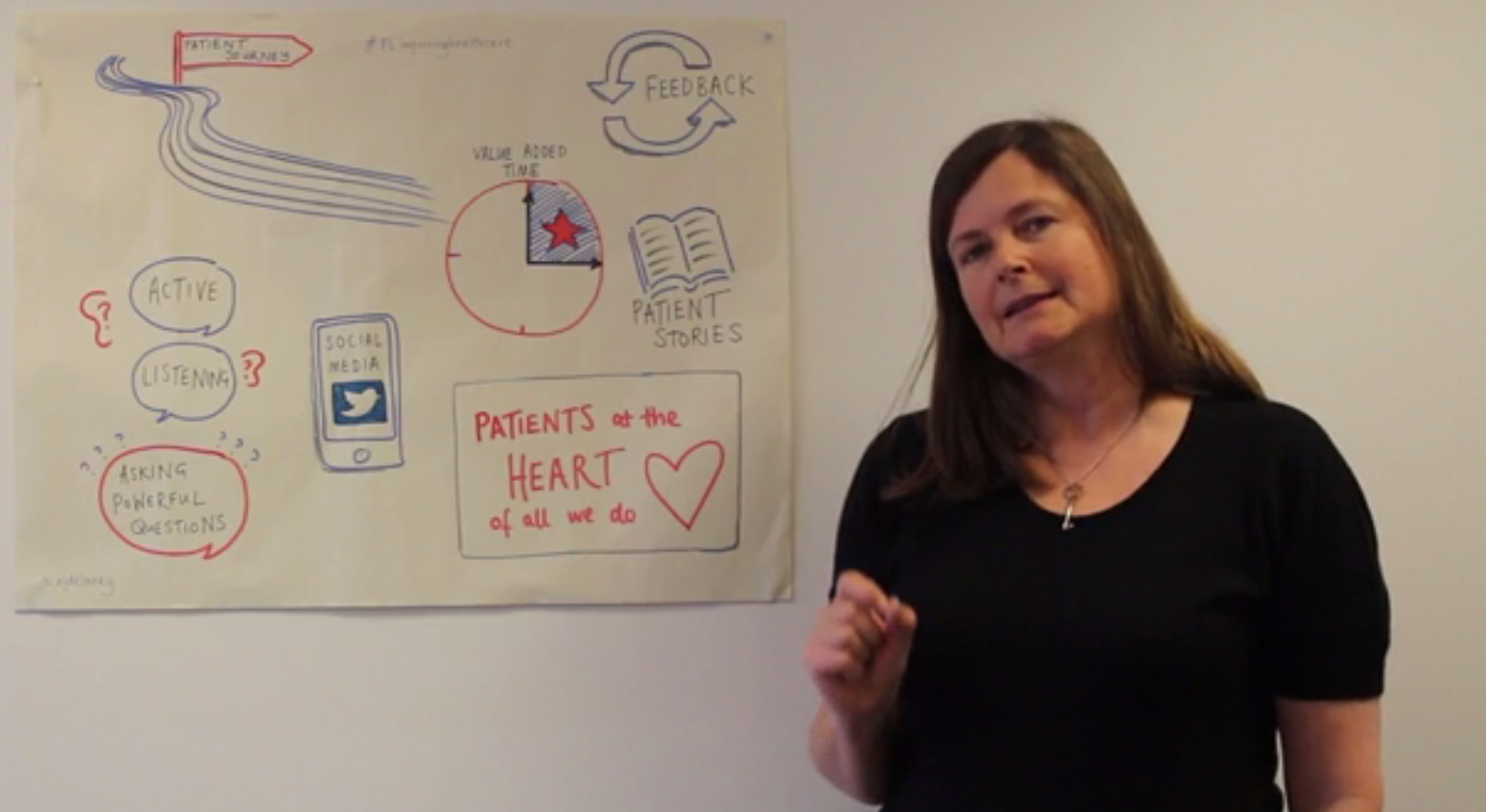
So here are eight, tried and tested ideas that might help improve the type of patient-focused care offered by your organisation:
1. Focus on the patient journey
An important element of QI is always to think about the patient journeys through your system. One simple, but effective, way to really get to know the patient journey is to experience it in ‘real time’, by asking permission to accompany a patient as they travel through your system. You will see and, more importantly feel, how they move through the care pathway. You will see how smooth, efficient and effective the care is and what really matters from the patient’s perspective. Often this process will help you to see things from a different perspective, noticing both the ‘flow’ through the system and ‘emotional touchpoints’ of the journey, the elements where the patient is pleased, frustrated, bored, vulnerable, empowered etc. This method enables you to collect powerful data and can assist you combine a process map of the patient journey with the experience of the journey.
2. Value added time
Once you have mapped the whole patient journey, you can start to ask a range of questions like:
“What parts of the journey really add value to the patient?”
“Is there any unnecessary duplication or waste?”
“Can we make the experience of the journey better?”
You can then ask both patients and staff what ideas they would suggest to speed up this process and eradicate unnecessary steps in the journey that don’t add value. You have then started a process of co-production of improvement ideas that can be tested using Plan Do Study Act cycles. This is a quick and effective method to reduce steps in the process and can also be used to improve patient experience and safety.
3. Ask for feedback
Every NHS organisation has processes in place to gain feedback from patients about their experience of care, like the Friends and Family Test. This can help to give organisational feedback. However, what happens if you are trying out a new improvement idea in your team or microsystem and just want some very quick and direct feedback from patients as part of your improvement measures?
There are really creative ways of obtaining immediate feedback at a microsystem level, such as in a busy outpatient clinics or wards.
For instance waiting rooms can be great environments for feedback and measuring patient experience using more engaging and unique metrics. A simple yet effective technique is to give either your patient or their relatives or carers a token and ask them to drop it into one of two jars in the waiting room as they exit. You can label the jars according to the question you want answered. For instance if you were aiming to improve the running time of the clinic you might ask “Did you wait more than 5 mins after your scheduled appointment time?” and put out two jars, one labelled “yes” and one labelled “no”. This simple feedback can help you see how you are doing.
For younger patients, we recently asked them to help us generate improvement ideas by providing drawings of magic wands to colour in. We then asked “If you could make our service better today by magic, what would you do?” The children loved this idea and were colouring and writing on their wands in no time. These ideas can them be taken forward to be tested.
This type of feedback is a great option for those of you who love to get creative, as the only limit here is your own imagination!
4. Share patient’s stories
Patient stories are a core element of QI techniques and should never be underestimated. Their experiences can be a powerful way to inspire change at all levels of an organisation from a busy clinic right up to the board. Use them wisely to get buy in and describe why change is needed. Here is one we recently developed at the West of England AHSN to explain why using the National Early Warning Scores can save people’s lives.
5. Get social!
Social media is a great way both to get feedback and to help test change ideas through crowdsourcing. Often people are really keen to help and you can reach a wider and more diverse audience who have a broad range of ideas. This is an effective way of seeking active engagement on how to improve both hospitals and/or care settings.
6. Be a fantastic listener
If you are leading improvement, don’t forget that you can improve yourself too! Ask yourself do you really and truly listen to people to understand what they are saying, even when it’s a difficult conversation to have? Or do you habitually listen to answer? Be brave and ask for feedback from colleagues and patients about their experience of you.
The art of active listening is crucial for QI leaders and it’s a skill that can be learnt and improved. An easy exercise to help you understand the power and importance of this skill is to find a friendly QI colleague and both take turns to tell each other something important while the other person tries as hard as they can not to listen. It’s a good technique to show how not listening to someone impacts on us emotionally.
7. Don’t underestimate the power of a question
If you unearth a patient experience issue in your team you can help to better understand it by using the ‘Five Whys’ technique. This is a very simple QI method based on asking “why?” five times to take you on a deep dive to the root cause of the issue. This can then help you see if this was an unfortunate ‘one-off’ variation to the norm or a systemic issue that will require wider improvement.
8. Appreciative Inquiry
Appreciative Inquiry is a technique developed by Cooperrider et al (2010). It can be used across an organisation or in a single team, for staff and patients, carers and families. It asks ‘appreciative’ questions about what’s working well and why. It is a strengths and asset led model where you actively seek to build on what you’re good at rather than ‘problem solve’ by looking only at deficits. This doesn’t mean that you don’t uncover things that need improvement; in fact it asks people to dream about what the organisation could look like in the future in order to continuously improve and transform.
I hope you have enjoyed reading these techniques, and are inspired to give one of them a go. I’d love to hear your ideas too so that together we can spread ideas about how to improve patient-centred care approach and leadership skills. I believe no matter what your role is in your healthcare environment, we are all leaders for improvement. Please feel free to tweet us at @annaburhouse or @weahsn with your suggestions.
Posted on April 5, 2017 by Anna Burhouse, Director of Quality, West of England AHSN


